Acoustic Basics - How does US travel interact with medium
How does US travels through a medium and transfer between media
a. Propagation velocity
b. Acoustic impedance
2. Reflection:
a. Impedance mismatch
b. Specular Pattern
c. Diffuse Pattern
3. Refraction
4. Attenuation
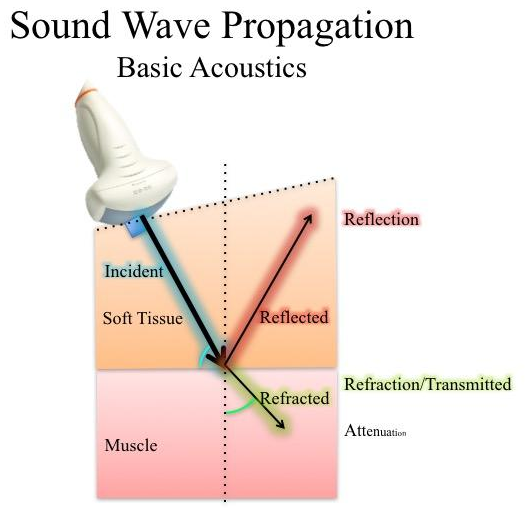
1. Sound Wave Propagation
The incident wave is the pulse that is emitted from the transducer. This diagram illustrates the types of propagation that we will be exploring.
For the purpose of discussion and illustration, each type of propagation is colour coded.
To understand how sound wave moves through a medium, we need to learn some basic physics:
a. Propagation velocity
b. Acoustic Impedance
The incident wave is the pulse that is emitted from the transducer. This diagram illustrates the types of propagation that we will be exploring.
For the purpose of discussion and illustration, each type of propagation is colour coded.
To understand how sound wave moves through a medium, we need to learn some basic physics:
a. Propagation velocity
b. Acoustic Impedance
a. Propagation Velocity:
speed of a pulse wave - this is described by the equation. As you can see, it is dependent on the characteristic of the tissue it is traversing through. In fact, US wave travels at a specific velocity in a specific medium, which implies the propagation velocity is constant for that medium.
The denser the medium, the closer are the particles to propagate the wave, therefore the velocity is higher.
However, when the medium is less dense, it is more difficult for the sparse particles to transmit the wave, therefore the velocity is lower.
The denser the medium, the closer are the particles to propagate the wave, therefore the velocity is higher.
However, when the medium is less dense, it is more difficult for the sparse particles to transmit the wave, therefore the velocity is lower.

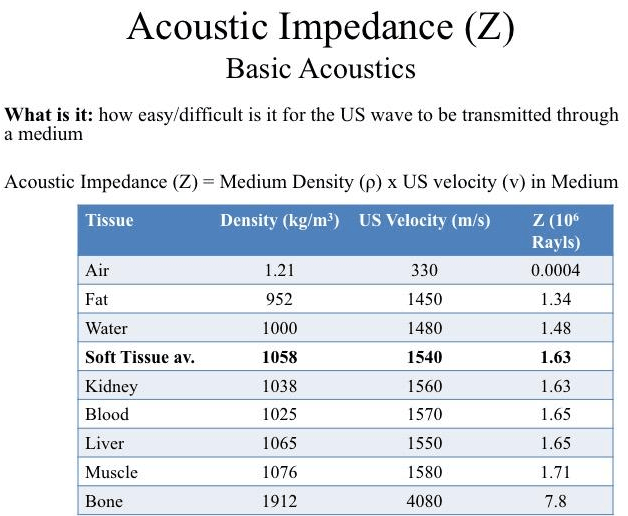
b. Acoustic Impedance
This table tabulates the medium specific propagation velocities for clinical ultrasound. As you can see, bone has a high Z. This means US propagates through it easily due to its relatively high density and, hence, rapidly at 4080m/s. Air, on the other hand, has a low density, so it has a low Z, therefore the propagating velocity is low.
A note, "Soft tissue" consists of multiple constituents, therefore an average is used. Its propagating velocity of 1540m/s is an important number as all US machines assume that US velocity is constant and fixed at 1540m/s in order to calculate distance. You may think that the differences are minor. For example, Fat's velocity of 1450m/s is only 90m/s slower than soft tissue, but this suffices to generate artifacts.
This table tabulates the medium specific propagation velocities for clinical ultrasound. As you can see, bone has a high Z. This means US propagates through it easily due to its relatively high density and, hence, rapidly at 4080m/s. Air, on the other hand, has a low density, so it has a low Z, therefore the propagating velocity is low.
A note, "Soft tissue" consists of multiple constituents, therefore an average is used. Its propagating velocity of 1540m/s is an important number as all US machines assume that US velocity is constant and fixed at 1540m/s in order to calculate distance. You may think that the differences are minor. For example, Fat's velocity of 1450m/s is only 90m/s slower than soft tissue, but this suffices to generate artifacts.
2. Reflection
Reflection is the principle propagation that allows diagnostic imaging with US, because when the pulse emits a pulse wave, the transducer then listens for an echo which the machine processes to form an image.
So we have a curvilinear probe, it is placed next to the soft tissue. When the the pulse wave strikes the interface between soft tissue and bone, part of that incident beam is reflected.
Reflection occurs when there is an Impedance Mismatch - at interfaces between media that possess different acoustic impedance.
Reflection is the principle propagation that allows diagnostic imaging with US, because when the pulse emits a pulse wave, the transducer then listens for an echo which the machine processes to form an image.
So we have a curvilinear probe, it is placed next to the soft tissue. When the the pulse wave strikes the interface between soft tissue and bone, part of that incident beam is reflected.
Reflection occurs when there is an Impedance Mismatch - at interfaces between media that possess different acoustic impedance.
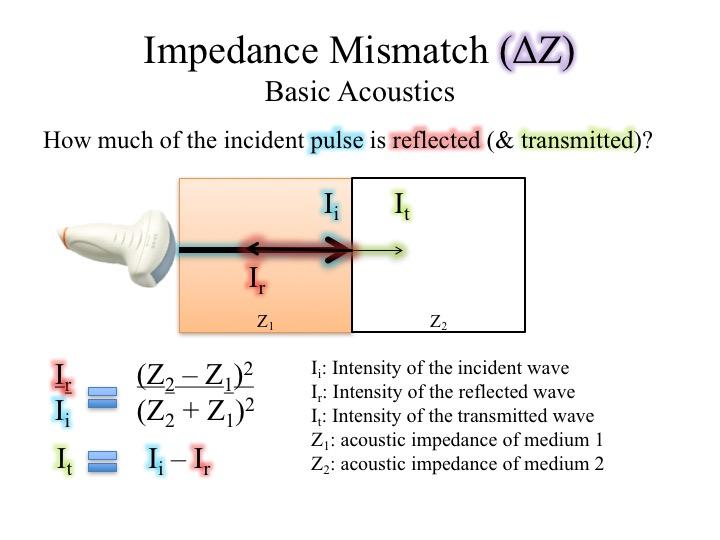
a. Impedance Mismatch
So how much is that incident wave reflected and transmitted? The diagram shows at the interface between medium 1 and 2, both a reflection wave and a transmission wave are generated.
Their respective intensities can be described by a simple relationships as shown.
Given the law of conservation of energy:
Ii = 1
Ii = Ir + It
Let's illustrate these relationships with some examples.
So how much is that incident wave reflected and transmitted? The diagram shows at the interface between medium 1 and 2, both a reflection wave and a transmission wave are generated.
Their respective intensities can be described by a simple relationships as shown.
Given the law of conservation of energy:
Ii = 1
Ii = Ir + It
Let's illustrate these relationships with some examples.
What happens when an incident pulse is to pass through a medium of relatively lower Z (ie. soft tissue) to a medium of relatively higher Z (ie. bone)?
In this scenario, an US pulse is to traverse from soft tissue to bone - like when you are scanning muscle and joints.
We plug in the respective Z values into the formula for which Ir = 0.43. This means that 43% of the incident wave will be reflected. Given conservation of energy, It = 0.57 which means 57% will be transmitted.
In this scenario, an US pulse is to traverse from soft tissue to bone - like when you are scanning muscle and joints.
We plug in the respective Z values into the formula for which Ir = 0.43. This means that 43% of the incident wave will be reflected. Given conservation of energy, It = 0.57 which means 57% will be transmitted.

What if we have the scenario where an incident pulse is to pass from a medium of relatively lower Z (ie. air) to a medium of relatively higher Z (ie. soft tissue)?
In this scenario, an US pulse is to traverse from air to soft tissue -- like when we scan without US gel.
We plug in the respective Z values into the formula for which Ir = 0.99. This means that 99% of the incident wave will be reflected. Given conservation of energy, It = 0.01 which means 1% will be transmitted.
Almost all of the Ii is reflected in this case, because the Impedance Mismatch is very high.
In this scenario, an US pulse is to traverse from air to soft tissue -- like when we scan without US gel.
We plug in the respective Z values into the formula for which Ir = 0.99. This means that 99% of the incident wave will be reflected. Given conservation of energy, It = 0.01 which means 1% will be transmitted.
Almost all of the Ii is reflected in this case, because the Impedance Mismatch is very high.

Now, if you apply US gel between the transducer and the soft tissue, what will happen to the propagation?
US Gel's Z is similar to water = 1.48. Hence, we have created a situation where the pulse wave will pass through a medium of relatively lower Z to a medium of relatively higher Z.
Ir = 0.002 = 0.2% will be reflected. It = 0.998 = 99.8% will be transmitted. You may, now, appreciate the importance of US gel application to improve diagnostic imaging.
Almost all of the Ii is transmitted in this case, because the Impedance Mismatch is very low.
US Gel's Z is similar to water = 1.48. Hence, we have created a situation where the pulse wave will pass through a medium of relatively lower Z to a medium of relatively higher Z.
Ir = 0.002 = 0.2% will be reflected. It = 0.998 = 99.8% will be transmitted. You may, now, appreciate the importance of US gel application to improve diagnostic imaging.
Almost all of the Ii is transmitted in this case, because the Impedance Mismatch is very low.

Let's take a look at another example whereby the an US pulse is to move between two media of very similar Z's. In this case, we have the US wave pass from fat to soft tissue.
Ir = 0.009 = 0.9% reflection.
It = 0.991 = 99.1% transmitted.
Again, just like the previous scenario, most of the Ii is transmitted.
Ir = 0.009 = 0.9% reflection.
It = 0.991 = 99.1% transmitted.
Again, just like the previous scenario, most of the Ii is transmitted.

This table summarizes the results of the four scenarios illustrated above.
Take Home Messages:
Take Home Messages:
- As Impedance Mismatch approaches 0, transmission increases yet reflection decreases
- As Impedance Mismatch deviates from 0, transmission decreases yet reflection increases
- When Impedance Mismatch is = 0, there is only transmission

Given the importance of the relationship between Acoustic Mismatch and Wave Propagation, we shall illustrate it again with the animation on the left
Take Home Messages:
Take Home Messages:
- As Impedance Mismatch approaches 0, transmission increases yet reflection decreases
- As Impedance Mismatch deviates from 0, transmission decreases yet reflection increases
- When Impedance Mismatch is = 0, there is only transmission
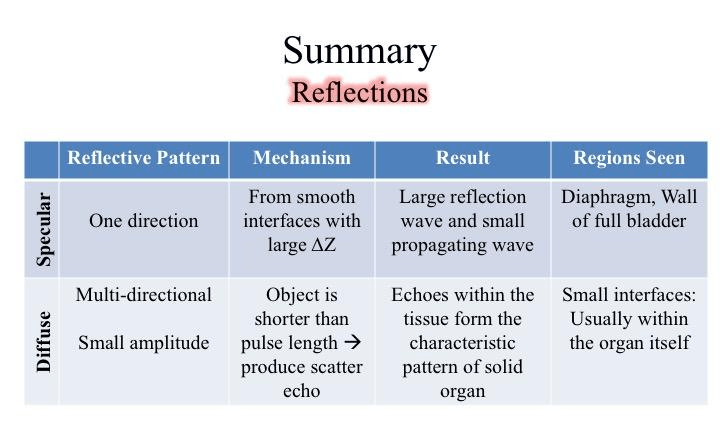
b. Specular and Diffuse Reflection
So far we have discussed about Reflection from the perspective of Acoustic Mismatch. To further build upon this concept, we shall add in Reflection direction and angle.
This introduces two reflective patterns: Specular Reflection and Diffuse Reflection.
So far we have discussed about Reflection from the perspective of Acoustic Mismatch. To further build upon this concept, we shall add in Reflection direction and angle.
This introduces two reflective patterns: Specular Reflection and Diffuse Reflection.
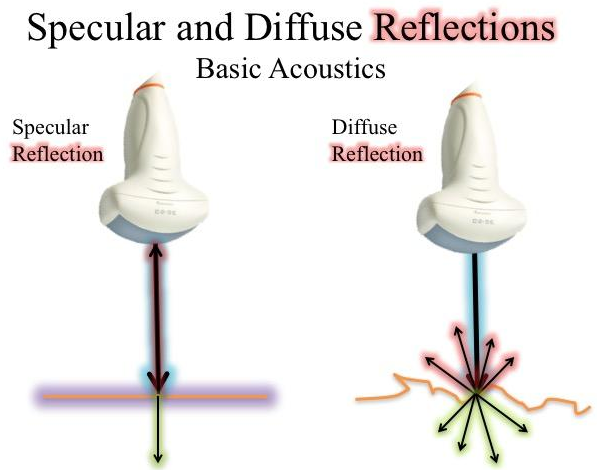
Specular Reflection:
When an incident pulse encounters a large smooth interface with ΔZ, the pulse will be reflected. The echo's intensity is proportional to the ΔZ of the two medium.
If the incident pulse reaches the interface at 90°, almost all of the generated echo will reflect to the transducer at the same angle. However, if the angle of incidence with the specular boundary is <90°, the echo will not return to the transducer, but reflected at an angle equal to the angle of incidence. The returning echo may potentially miss the transducer and not be detected. This is of practical importance, and it explains why it may be difficult to image a needle when it is is inserted at a very steep angle.
If the incident pulse reaches the interface at 90°, almost all of the generated echo will reflect to the transducer at the same angle. However, if the angle of incidence with the specular boundary is <90°, the echo will not return to the transducer, but reflected at an angle equal to the angle of incidence. The returning echo may potentially miss the transducer and not be detected. This is of practical importance, and it explains why it may be difficult to image a needle when it is is inserted at a very steep angle.
Diffuse Reflection:
If the incident pulse encounters reflectors whose dimensions are smaller than the pulse wavelength, or when the pulse encounters an irregular tissue interface, scattering occurs. In this case, multiple echoes are be generated at various angles which reduce the intensity of individual reflections. However, scattering does allow some echo to return to the transducer regardless of the angle of incidence.
Most biologic tissues appear on US images as though they are filled with tiny little dots. These speckle signals that you see provides a visible texture for solid organs like the liver or muscle. They are created by the many small interfaces within the organ.
Most biologic tissues appear on US images as though they are filled with tiny little dots. These speckle signals that you see provides a visible texture for solid organs like the liver or muscle. They are created by the many small interfaces within the organ.
Take Home Messages:
- Specular reflection: unidirectional reflection and occurs at large and smooth surfaces such as the diaphragm and bladder wall
- Diffuse reflection: produces the characteristic tissue texture one sees within the organ itself
3. Refraction
It refers to the change in direction (angle) and propagating speed of the incident pulse when it strikes an interface at an oblique angle. Because sound frequency is constant during this transmission process, the wavelength has to change in order to accommodate the difference in propagation velocity specific to the tissues. This, also, results in a redirection of the sound pulse as it passes through the interface.
It refers to the change in direction (angle) and propagating speed of the incident pulse when it strikes an interface at an oblique angle. Because sound frequency is constant during this transmission process, the wavelength has to change in order to accommodate the difference in propagation velocity specific to the tissues. This, also, results in a redirection of the sound pulse as it passes through the interface.

Practical Point:
Refraction is one of the important causes of incorrect localization of a structure on an ultrasound image. Because the speed of sound is low in fat (approximately 1,450 m/s) and high in soft tissues (approximately 1,540 m/s), refraction artifacts are most prominent at fat/soft tissue interfaces.
Here are three scenarios to illustrate refraction.
Scenario 1: incident pulse traverses from Z1 to Z2 where Z1>Z2: Refraction angle<Incident angle.
Scenario 2: incident pulse traverses from Z1 to Z2 where Z2>Z1: Refraction angle >Incident angle.
Scenario 3: incident pulse strikes the interface at a 90°. The refracted wave will be at 90°.
Take Home Messages:
Scenario 1: incident pulse traverses from Z1 to Z2 where Z1>Z2: Refraction angle<Incident angle.
Scenario 2: incident pulse traverses from Z1 to Z2 where Z2>Z1: Refraction angle >Incident angle.
Scenario 3: incident pulse strikes the interface at a 90°. The refracted wave will be at 90°.
Take Home Messages:
- occurs when the incident pulse strikes an interface at an oblique angle
- changes the direction of the pulse wave

4. Attenuation
As an US wave traverses through a medium/media, its amplitude reduces. The reason for why this happens is that US energy is lost to its environment through three mechanisms:
As an US wave traverses through a medium/media, its amplitude reduces. The reason for why this happens is that US energy is lost to its environment through three mechanisms:
- absorption
- reflection
- refraction
Attenuation is affected by three factors:
So air dissipates lots of energy compared to water.
- Attenuation coefficient (α): an intrinsic property of a medium as tabulated
- Distance the US wave traveled
- Frequency of the US pulse
So air dissipates lots of energy compared to water.
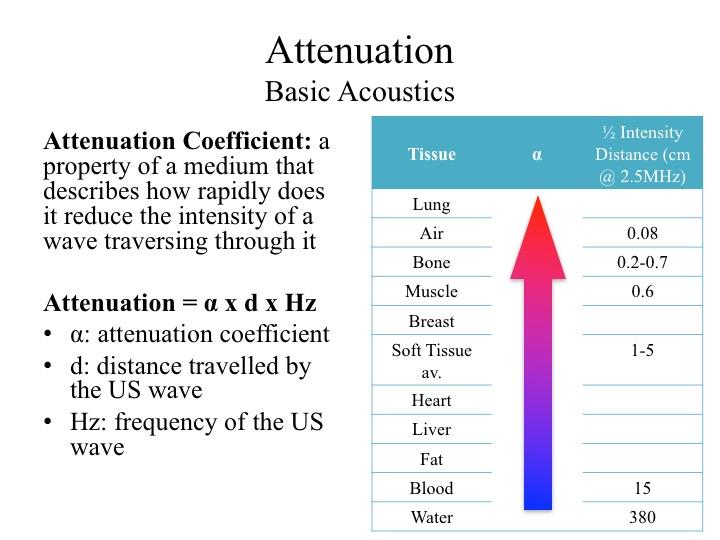
If we plot attenuation to distance traveled and frequency of the pulse wave, this is the result. On the Y-axis is intensity and X-axis is distance traveled by the US pulse.
Suppose we emit 3 US pulses of escalating frequencies into soft tissue, the following are the key observations:
Suppose we emit 3 US pulses of escalating frequencies into soft tissue, the following are the key observations:
- the lower the MHz, the less the attenuation
- the higher the MHz, the more the attenuation

Practical Point:
- For deep structures, low MHz maybe preferable because the intensity of the wave will be less attenuated - having enough energy to travel to-&-fro for image processing
- For highly attenuating tissues, use low MHz
Take Home Messages:
- Propagating Velocity of a pulse wave is tissue specific
- When an incident pulse wave strikes an interface between two medium with different Acoustic Impedance (Acoustic Mismatch), the beam may reflect or refract
- Reflection has two types: Specular and Speckled
- Refraction changes angle of the incident pulse when it strikes an Acoustic Mismatch interface at an oblique angle
- Energy/Intensity of an US beam is dissipated through the process of attenuation