Vascular Access - Basics - Needle Imaging
Needle Imaging
What does the needle look like under ultrasound?
1. Needle Anatomy
2. Angiocath versus Steel Needle
3. Angle of Insonation
What does the needle look like under ultrasound?
1. Needle Anatomy
2. Angiocath versus Steel Needle
3. Angle of Insonation
1. Needle Anatomy
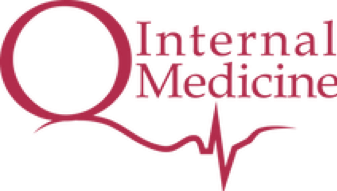
The relevant needle anatomy to be aware of for point of care ultrasound is the tip and the shaft. For a steel needle, both the tip and the shaft are exposed with nothing covering them. For the angiocath, the tip is exposed but the shaft is covered by the cathether.
When the ultrasound contacts the needle, it generates an hyperechoic signal on the screen. The tip may yield a visible ringdown artifact whereas the shaft will just look hyperechoic on the monitor. The catheter will, however, attenuate some of that ultrasound signal making it harder to see with ultrasound.
The relevant needle anatomy to be aware of for point of care ultrasound is the tip and the shaft. For a steel needle, both the tip and the shaft are exposed with nothing covering them. For the angiocath, the tip is exposed but the shaft is covered by the cathether.
When the ultrasound contacts the needle, it generates an hyperechoic signal on the screen. The tip may yield a visible ringdown artifact whereas the shaft will just look hyperechoic on the monitor. The catheter will, however, attenuate some of that ultrasound signal making it harder to see with ultrasound.
So how does the needle tip and body look like under ultrasound in the short axis view?
The needle tip vibrates when the ultrasound hits it which will generates a reverberation artifact just inferior to the tip. The artifact is characterized by short horizontal lines that are stacked on top of each other. The top two static photos illustrate how the tip and artifact look like in different environments. When the tip is situated in echoic tissue, the artifact is not easily seen. However, when the tip is in the vessel lumen, the reverberation artifact it more distinct as the anechoic or hypoechoic background accentuates the hyperechoic artifact.
In terms of the needle body, it manifests as an hyperechoic point with no reverberation artifact.
The needle tip vibrates when the ultrasound hits it which will generates a reverberation artifact just inferior to the tip. The artifact is characterized by short horizontal lines that are stacked on top of each other. The top two static photos illustrate how the tip and artifact look like in different environments. When the tip is situated in echoic tissue, the artifact is not easily seen. However, when the tip is in the vessel lumen, the reverberation artifact it more distinct as the anechoic or hypoechoic background accentuates the hyperechoic artifact.
In terms of the needle body, it manifests as an hyperechoic point with no reverberation artifact.
So how does the needle tip and body look like under ultrasound in the long axis view. the ring-down artifact maybe visible at the needle tip depending on the angle of insonation to the tip.
The static photos illustrate how the tip and the anechoic region inferior to the needle body due to attenuation of the US by the metal.
In terms of the needle body, the entire body will be visualized.
The static photos illustrate how the tip and the anechoic region inferior to the needle body due to attenuation of the US by the metal.
In terms of the needle body, the entire body will be visualized.
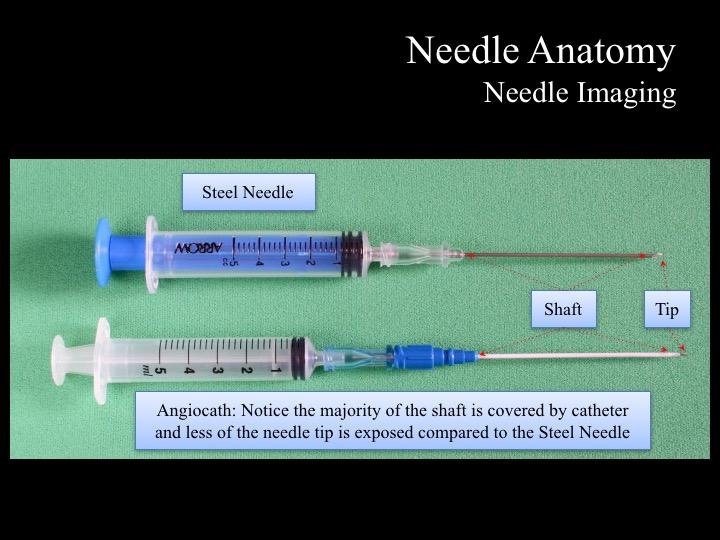
2. Angiocath vs Steel Needle
The previous two slides are images of the steel needle traversing through tissues in the short and long axis. Now, let’s compare them to the Angiocath where there is a catheter sheath around the the shaft. Take a look at the static images on our left here. The images on the top row are taken for Angiocath, and the bottom row for Steel Needle.
Notice for the Angiocath, the it is echoic rather than hyperechoic compared to the Steel. If you image the Angiocath's body, it is not to spot it from the surrounding tissues due to similar echogenicity. However, the needle tip is still quite hyperechoic as shown. So it is very important to keep imaging the needle tip if you are using the angiocath for catheterization.
The previous two slides are images of the steel needle traversing through tissues in the short and long axis. Now, let’s compare them to the Angiocath where there is a catheter sheath around the the shaft. Take a look at the static images on our left here. The images on the top row are taken for Angiocath, and the bottom row for Steel Needle.
Notice for the Angiocath, the it is echoic rather than hyperechoic compared to the Steel. If you image the Angiocath's body, it is not to spot it from the surrounding tissues due to similar echogenicity. However, the needle tip is still quite hyperechoic as shown. So it is very important to keep imaging the needle tip if you are using the angiocath for catheterization.
3. Angle of Insonation
The angle of insonation is best appreciated in the long axis view. Here I am inserting the needle at various angles of entry. Take note of the echogenicity and the definition of the needle tip and body. At a shallow angle of entry, everything looks quite well defined, but as the needle starts penetrating at steeper angles, everything seems more fuzzy and hazy. When the US beam is perpendicular to the structure of interest, the reflection from the structure is maximized to generate the clearest image. As the transducer insonates at angles more and more parallel to the needle, less and less is reflected back, therefore the resolution of the structures fades. This, also, holds true for short axis – especially the short axis view.
The angle of insonation is best appreciated in the long axis view. Here I am inserting the needle at various angles of entry. Take note of the echogenicity and the definition of the needle tip and body. At a shallow angle of entry, everything looks quite well defined, but as the needle starts penetrating at steeper angles, everything seems more fuzzy and hazy. When the US beam is perpendicular to the structure of interest, the reflection from the structure is maximized to generate the clearest image. As the transducer insonates at angles more and more parallel to the needle, less and less is reflected back, therefore the resolution of the structures fades. This, also, holds true for short axis – especially the short axis view.
Key Messages:
- Short axis: Needle tip and body BOTH look very similar - the tip may produce a ringdown artifact
- Long axis: Advantage of easily discriminating between the tip and body
- The needle is best visualized when the angle of insonation is perpendicular to the needle