Vascular Access - Basics - Knobology
Knobology
Vascular imaging and, especially, real-time US needle guidance demands their own settings in order to optimize resolution and performance.
1. Probe Selection
2. Knobology Optimization
Vascular imaging and, especially, real-time US needle guidance demands their own settings in order to optimize resolution and performance.
1. Probe Selection
2. Knobology Optimization
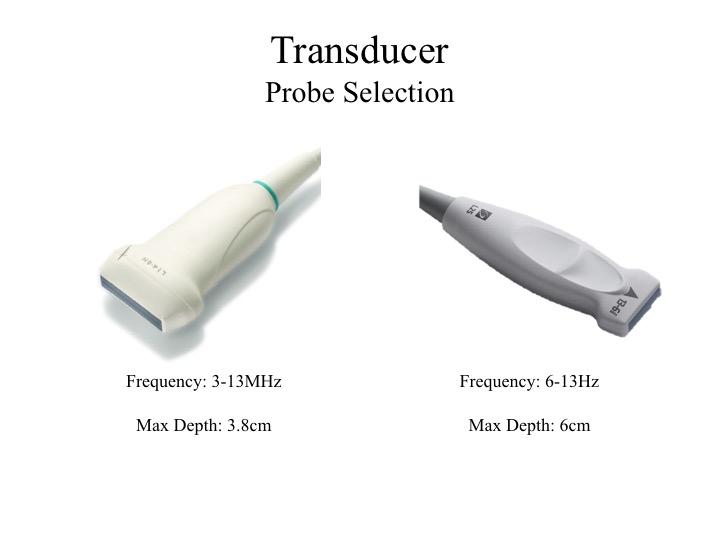
1. Probe Selection
The vasculature relevant to internal medicine bedside procedures are relatively superficial structures, therefore we need a transducer that best image this level of depth.
The Linear probe is the probe of choice for this indication given its high frequency bandwidth which yields high resolution images for superficial structures. The footprint geometry is, also, suited for the regions to be assessed and for real-time needle guidance.
The vasculature relevant to internal medicine bedside procedures are relatively superficial structures, therefore we need a transducer that best image this level of depth.
The Linear probe is the probe of choice for this indication given its high frequency bandwidth which yields high resolution images for superficial structures. The footprint geometry is, also, suited for the regions to be assessed and for real-time needle guidance.
2. Knobology Optimization
a. Depth to Visual Real-Estate Ratio
As you change the depth an image, the so called visual real estate changes. As we increase the depth, the image on the screen gets narrower; and as we reduce the depth, the image on the screen gets wider. You can appreciate that the image on the lower right hand corner that was taken at 5.1cm looks narrower than the other image taken at 1.9cm. Well, despite there appears to be a discrepancy in width, the distance between A and B are equal because the same width of tissue is being scanned. However, B just looks narrower because the monitor has to accommodate for the deeper depth that has been selected. So always maximize your visual real estate. If you do not need to look that deep, just set the depth sufficiently deep to view the structure of interest.
a. Depth to Visual Real-Estate Ratio
As you change the depth an image, the so called visual real estate changes. As we increase the depth, the image on the screen gets narrower; and as we reduce the depth, the image on the screen gets wider. You can appreciate that the image on the lower right hand corner that was taken at 5.1cm looks narrower than the other image taken at 1.9cm. Well, despite there appears to be a discrepancy in width, the distance between A and B are equal because the same width of tissue is being scanned. However, B just looks narrower because the monitor has to accommodate for the deeper depth that has been selected. So always maximize your visual real estate. If you do not need to look that deep, just set the depth sufficiently deep to view the structure of interest.

b. Colour Doppler
Doppler can be used to help differentiating between vasculature vs non-vascular mimics, and, also, distinguishing between artery vs vein.
θ: Angle of Insonation
Colour Signal - What does it mean?
By default and convention:
Doppler can be used to help differentiating between vasculature vs non-vascular mimics, and, also, distinguishing between artery vs vein.
θ: Angle of Insonation
Colour Signal - What does it mean?
By default and convention:
- Red: flow is moving TOWARDS the transducer
- Blue: flow is moving AWAY from the transducer

Clip i. Arterial Doppler Signal and Angle of Insonation
- Top: θ is perpendicular to flow - no signal
- Bottom: θ is directed towards flow - pulsatile red signal
Clip ii. Venous Doppler Signal and Angle of Insonation
- Top: θ is perpendicular to flow - no signal
- Bottom: θ is directed away flow - pulsatile blue signal
c. Frequency Selection
The Frequency emitted by the probe can be further refined by selecting a specific region along the Bandwidth spectrum.
The higher the Frequency, the better the spatial resolution. However, you will notice that the temporal resolution fades.
However, if you use the lower Frequency, temporal resolution improves but at the expense of spatial resolution.
In general, a middle of the Bandwidth yields the best of both worlds. However, compare and contrast to find the setting that best suit your needs.
The Frequency emitted by the probe can be further refined by selecting a specific region along the Bandwidth spectrum.
The higher the Frequency, the better the spatial resolution. However, you will notice that the temporal resolution fades.
However, if you use the lower Frequency, temporal resolution improves but at the expense of spatial resolution.
In general, a middle of the Bandwidth yields the best of both worlds. However, compare and contrast to find the setting that best suit your needs.

d. Compound Imaging Mode:
Advantage:
Disadvantage:
Advantage:
- Enhances needle imaging
- Tissue imaging and speckle artifacts are optimized
Disadvantage:
- Reduces temporal resolution

e. Temporal Resolution
Real-Time ultrasound guided procedure requires:
Real-Time ultrasound guided procedure requires:
- HIGH temporal resolution: so you can track needle movement
- GOOD spatial resolution: so you can see the borders of each structure
Key Message:
- Optimize the settings to achieve a balance between spatial and temporal resolutions
- Compare and contrast different settings for the optimal imaging performance
- Doppler: No signal will be detected if the angle of insonation is perpendicular to flow
- Doppler: Red colour does not mean Arterial Flow, and Blue colour does not mean Venous Flow