Pleural Effusion and Thoracentesis - Evidence
Pleural Effusion - Evidence
a. Why use PoCUS for detecting pleural effusion
b. Spine Sign
c. US Guided Thoracentesis
a. Why use PoCUS for detecting pleural effusion
b. Spine Sign
c. US Guided Thoracentesis
a. Why use PoCUS for detecting pleural effusion
We know that physical exam for pleural effusion has its limitation particularly when the patient is obese, or unable to sit up properly to examine the posterior aspect of the thorax.
The advent of CXR has revolutionized thoracic diagnoses -- pleural effusions can be seen so long as the film acquisition is proper and there is sufficient volume of fluid in the pleural space. For a PA upright CXR, costophrenic blunting manifests when >300mL accumulate in the most dependent region of the pleural space. In the lateral upright CXR, much smaller effusion can be detected. However, in practice, inpatients are unable to stand to obtain a proper PA and lateral CXR. Often a bedside AP CXR is obtained with the patient in a semi-supine position. This dramatically lowers the sensitivity and specificity for pleural effusion.
Ultrasound has been repeated show to out perform CXR, regardless of the technique used, when referenced to the accepted gold standard -- CT thorax (see below).
We know that physical exam for pleural effusion has its limitation particularly when the patient is obese, or unable to sit up properly to examine the posterior aspect of the thorax.
The advent of CXR has revolutionized thoracic diagnoses -- pleural effusions can be seen so long as the film acquisition is proper and there is sufficient volume of fluid in the pleural space. For a PA upright CXR, costophrenic blunting manifests when >300mL accumulate in the most dependent region of the pleural space. In the lateral upright CXR, much smaller effusion can be detected. However, in practice, inpatients are unable to stand to obtain a proper PA and lateral CXR. Often a bedside AP CXR is obtained with the patient in a semi-supine position. This dramatically lowers the sensitivity and specificity for pleural effusion.
Ultrasound has been repeated show to out perform CXR, regardless of the technique used, when referenced to the accepted gold standard -- CT thorax (see below).

PoCUS' higher sensitivity for pleural effusion is not surprising as the acquisition technique images the most dependent region of the thorax -- where fluid accumulates with gravity. In addition, even if the patient is in supine, PoCUS can still detect the fluid so long as it is not a trace amount. In comparison to CXR, in the supine position, the effusion layers out and the hemithorax may appear more opaque.
b. Spine Sign
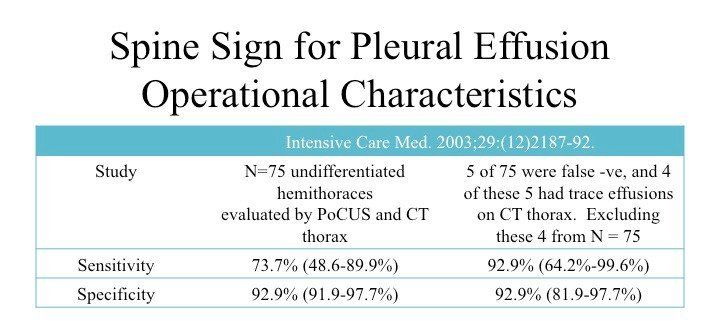
This was the original study that described and evaluated the operational characteristics of the Spine Sign. It performed surprisingly well so long as the effusion was not too small (the study did not define what was meant by "trace effusion").
However, even if PoCUS cannot detect trace effusions, in the context of elucidating dyspnea NYD, such a miniscule pleural collection in-of-itself cannot account for the symptomatic complaint. Hence, the lack of sensitivity for trace effusion with PoCUS is not clinically significant.
Other than the size of the effusion, the sensitivity of this sign, also, depends on whether the fluid may gravitate towards the most dependent region of the thorax. Having the patient at Trendelenburg or erect position allows the pleural fluid to gravitate to the most dependent region of the pleural space will improve diagnostic yield -- especially for small effusions which may layer out in supine positions which renders it much harder to detect. Of course, loculated effusions in other regions of the thorax, Zone 2 for example, will not be detected via this sonographic sign.
However, even if PoCUS cannot detect trace effusions, in the context of elucidating dyspnea NYD, such a miniscule pleural collection in-of-itself cannot account for the symptomatic complaint. Hence, the lack of sensitivity for trace effusion with PoCUS is not clinically significant.
Other than the size of the effusion, the sensitivity of this sign, also, depends on whether the fluid may gravitate towards the most dependent region of the thorax. Having the patient at Trendelenburg or erect position allows the pleural fluid to gravitate to the most dependent region of the pleural space will improve diagnostic yield -- especially for small effusions which may layer out in supine positions which renders it much harder to detect. Of course, loculated effusions in other regions of the thorax, Zone 2 for example, will not be detected via this sonographic sign.
c. US Guided Thoracentesis
Iatrogenic pneumothorax as a complication following a thoracentesis has the highest rate of procedural complication in comparison to other common procedures (eg. central venous catheterization, paracentesis) performed by Internal Medicine. A systematic review and meta-analysis in 2010 by Gordon et al demonstrated the following:
Iatrogenic pneumothorax as a complication following a thoracentesis has the highest rate of procedural complication in comparison to other common procedures (eg. central venous catheterization, paracentesis) performed by Internal Medicine. A systematic review and meta-analysis in 2010 by Gordon et al demonstrated the following:
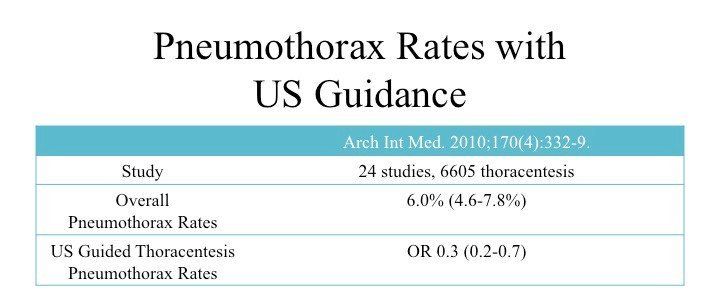
The complication rate is quite high at 6% for a pneumothorax following thoracentesis. However, with sonographic guidance, the odds of such a complication is 0.3 -- the risk is decreased by ~66%.
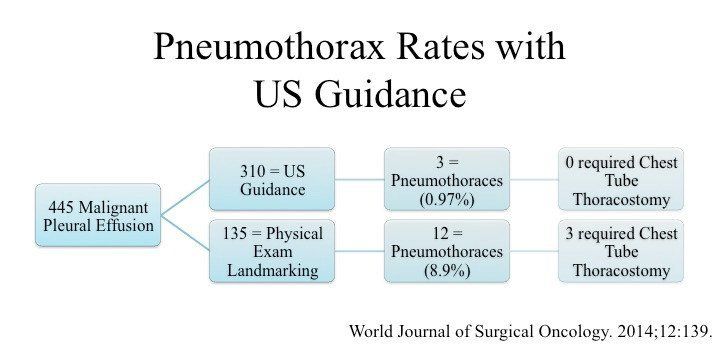
Other studies have demonstrated similar findings. In a 2014 retrospective study, Cavanna et al.
showed that ultrasound guided thoracentesis significantly reduced the pneumothorax rates: 0.97% vs 8.9%.
Of course, ultrasound guidance is only as good as the expertise of the operator. You need to know what you are looking
at
in order to landmark the correct site to insert the needle.
Take Home Messages:
- PoCUS is superior to physical exam and CXR in detecting pleural effusion
- Spine Sign has good operational characteristics provided that the effusion is not loculated at independent regions in the thorax
- Sonographic guidance reduces iatrogenic pneumothorax post-thoracentesis