Pleural Effusion and Thoracentesis - Pleural Effusion
Pleural Effusion
What will you be seeing on the monitor? We shall explore some of fundamental and commonly encountered sonographic features. They will serve as building blocks to help you elucidate other signs you may encounter.
1. Effusion appearance
1. Effusion Appearance:
- Fluid: spectrum from Anechoic (Black) to Echoic (Shades of grey and white)
- Non-Fluid Matters: Atelectatic lung, Fibrin, Particulates
Figure 2.
Echogenic material in the pleural space imaged from RZ4 of a loculated & gelatenous empyema.

Figure 3. Effusion with a spectrum of echocogenic material in the pleural space imaged from a patient with an gaseous empyema.

Figure 4. Echogenic effusion see at LZ4 from a patient in active CHF though fluid analysis was consistent with transudate.

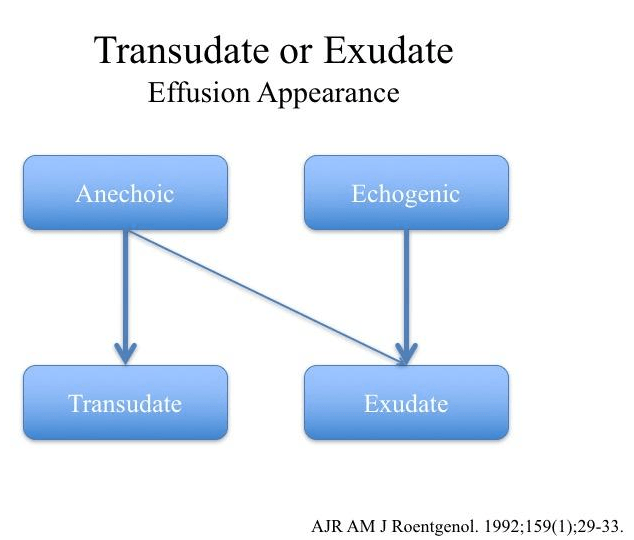
So does the effusion appearance predict whether the fluid is a transudate versus an exudate?
A study in 1992 compared the sonographic images against their respective pleural fluid analysis by Light’s criteria. The study demonstrated that the all echogenic effusions were exudative. However, despite the majority anechoic effusions are transudate, a small number turned out to exudative.
Of course, always interpret your image in conjunction with the clinical context.
A study in 1992 compared the sonographic images against their respective pleural fluid analysis by Light’s criteria. The study demonstrated that the all echogenic effusions were exudative. However, despite the majority anechoic effusions are transudate, a small number turned out to exudative.
Of course, always interpret your image in conjunction with the clinical context.
a. Mirror Artifact & Spine Sign
As a quick review, Mirror Artifact and Spine Sign are both used to help infer whether something other than air (eg. fluid, solid) is in the pleural space.
When an effusion is present: (see Video)
As a quick review, Mirror Artifact and Spine Sign are both used to help infer whether something other than air (eg. fluid, solid) is in the pleural space.
When an effusion is present: (see Video)
- Mirror Artifact: will be Mitigated
- Spine Sign: the portion of the spine CRANIAL to the diaphragm will become visible
These signs are useful for answering "Is there a pleural effusion?" especially when the patient is in a dependent position. However, it is NOT
good at detecting loculated effusions distal to Z4.
In this video imaged from RZ4, the spine is clearly visible cranial to the diaphragm. This suggests that there is something in the pleural space in the region being scanned.
What about the Mirror Artifact? The material in the pleural space appears similar to the liver that is opposite of the diaphragm. So is this a Mirror Artifact?
The answer is no. This is because if a true Mirror Artifact is present, the Spine Sign will be negative (Spine cranial to the diaphragm will not be visible).
What about the Mirror Artifact? The material in the pleural space appears similar to the liver that is opposite of the diaphragm. So is this a Mirror Artifact?
The answer is no. This is because if a true Mirror Artifact is present, the Spine Sign will be negative (Spine cranial to the diaphragm will not be visible).
b. Fibrin
In this video, it exhibits floating, wavy string-like structures are sometimes seen within a pleural effusion. These are fibrin strands, and their presence suggest an exudative fluid composition and possibly the presence of loculation.
If you see slither structures such as these floating in the effusion, ENSURE you sweep the entire structure to differentiate whether it is fibrin versus an atelectactic lung imaged at a thin cut.
In this video, it exhibits floating, wavy string-like structures are sometimes seen within a pleural effusion. These are fibrin strands, and their presence suggest an exudative fluid composition and possibly the presence of loculation.
If you see slither structures such as these floating in the effusion, ENSURE you sweep the entire structure to differentiate whether it is fibrin versus an atelectactic lung imaged at a thin cut.
c. Plankton Sign
Just like plankton floating in the sea, this sign refers to when particulate matters are visibly churning in the pleural fluid.
Usually, this findings suggest the presence of an exudative effusion.
Just like plankton floating in the sea, this sign refers to when particulate matters are visibly churning in the pleural fluid.
Usually, this findings suggest the presence of an exudative effusion.
d. Atelectactic Lung
As the external pressure of a pleural effusion progressively compress on the lung, more and more air is displaced from its air-space. Consequently, the lung becomes sufficient dense to develop an acoustic impedance similar to tissue - allowing it to be imaged.
The size and shape of an atelectatic lung varies depending on the magnitude of the external force, whether air flow is still present, and the imaging cut.
Here is an atelectacic lung that is severely compressed by a large effusion. No air bronchogram is visible implying there is no/minimal air flow into the lung.
As the external pressure of a pleural effusion progressively compress on the lung, more and more air is displaced from its air-space. Consequently, the lung becomes sufficient dense to develop an acoustic impedance similar to tissue - allowing it to be imaged.
The size and shape of an atelectatic lung varies depending on the magnitude of the external force, whether air flow is still present, and the imaging cut.
Here is an atelectacic lung that is severely compressed by a large effusion. No air bronchogram is visible implying there is no/minimal air flow into the lung.
In this particular video taken from LZ6 of a patient with severe pancreatitis, an anechoic effusion is present In addition, there appears to be echoic material just layering the diaphragm.
Initially, it was thought to be echogenic material gravitating to the most dependent part of the pleural space - costodiaphragmatic recess. However, as the pleural space and "material" were further imaged, the latter was noted to be an atelectactic lung adhered to the diaphragm.
Initially, it was thought to be echogenic material gravitating to the most dependent part of the pleural space - costodiaphragmatic recess. However, as the pleural space and "material" were further imaged, the latter was noted to be an atelectactic lung adhered to the diaphragm.
Let's take a look what happens to an atelectatic lung pre- and post-therapeutic thoracentesis.
Here we have a sizeable anechoic effusion with notable fibrinous material attached to the visceral pleura. The lung is well compressed with virtually adynamic air bronchograms - note the minimal movement of the echoic signals throughout this video despite the fact that the patient is actively inspiring and expiring.
Here we have a sizeable anechoic effusion with notable fibrinous material attached to the visceral pleura. The lung is well compressed with virtually adynamic air bronchograms - note the minimal movement of the echoic signals throughout this video despite the fact that the patient is actively inspiring and expiring.
1.5L of clear serous fluid was drained from the effusion, and the fluid pocket was re-imaged at the same window.
Clearly, the fluid pocket is smaller, therefore the lung occupies more of the pleural space. Also, notice the air bronchograms are much more dynamic than before - the echoic signals move all the way to the periphery of the lung due to improved air flow as external pressure is relieved.
Clearly, the fluid pocket is smaller, therefore the lung occupies more of the pleural space. Also, notice the air bronchograms are much more dynamic than before - the echoic signals move all the way to the periphery of the lung due to improved air flow as external pressure is relieved.
3. Mimic
This clip was taken from left zone 4. Notice that there is a curtain sign; and below the curtain, there is fluid collection with particulates inside. One would think this maybe a complex pleural effusion.
However, notice that this collection has a wall. This is, in fact, a distended and fluid filled stomach.
Take Home Messages:
- Anechoic effusion suggests a simple effusion - likely transudative
- Echogenic effusion, or presence of fibrin/particulate matters suggest a complicated effusion - likely exudative
- Atelectactic lung vary in appearance
- The degree of air flow limitation into the compressed lung can be inferred from dyanmic air bronchogram assessment