Lung Parenchyma - Case Illustration
Case 1.
31M with known medical history presented for routine check up.
Case 2.
46F with chronic graft versus host disease of her lungs developed acute on chronic SOB secondary to PCP pneumonia. Similar scans were acquired throughout her thorax.
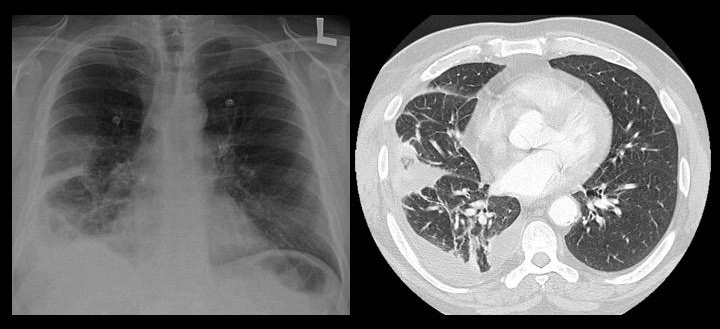
Case 3. 60M presented with acute dyspnea associated with right lateral pleurisy who was found to be hypoxic and septic.
CXR and CT chest demonstrated segmental parenchymal consolidation and a small effusion.
CXR and CT chest demonstrated segmental parenchymal consolidation and a small effusion.
The final diagnosis was pneumosepsis secondary to Streptococcus pneumoniae. The effusion analysis was consistent with a complicated parapneumonic effusion.
Before you scroll down for the sonographic images, what do you think it will show?
Clip 3a.
Take note the Fractal line demarcates the border between segmental consolidation and aerated parenchyma. The pleural line (hyperechoic line resulting from the apposition of the visceral and parietal pleura) is no longer visible as the VPPI is separated by an effusion. The Lung Line is the margins (visceral pleura) of the lung parenchyma, but it is NOT echoic.
Clip 3b.
This is imaged from another angle of the right lower thorax. Same findings are found. However, some B-lines are noted to be arising from the Lung Line. The air space in this region of lung is filled with exudate, but ONLY partially, as B-lines are seen instead of consolidation.
Case 4. 80F presented initially with fever who requiring 6L oxygen rapidly deteriorated necessitating a non-rebreather mask.
Unfortunately, physical exam was non-contributory due to obesity, and the CXR was rather poor in quality.
Thoracic PoCUS was performed aid elucidating the cause for her acute hypoxia.
Unfortunately, physical exam was non-contributory due to obesity, and the CXR was rather poor in quality.
Thoracic PoCUS was performed aid elucidating the cause for her acute hypoxia.

Thoracic PoCUS revealed A-lines and pleural sliding in all zones except for Z4 bilaterally. Lots of B-lines were visible in these regions.
The greater the number of B lines (and, therefore, the closer they are to each other), the more severe the interstitial syndrome.
In this case of congestive heart failure, the high number of B lines suggests the pulmonary edema is severe: alveolar edema in conjunction to interstitial edema.
The greater the number of B lines (and, therefore, the closer they are to each other), the more severe the interstitial syndrome.
In this case of congestive heart failure, the high number of B lines suggests the pulmonary edema is severe: alveolar edema in conjunction to interstitial edema.
Case 5.
74M heavy smoker presented with weight loss and chest pain localized to the right upper thorax. No breath sound was audible at the RUL, and this region was dull to percussion. At the time, CXR was pending, therefore a thoracic PoCUS was performed.
Case 6.
33F who was 4 weeks post-partum presented with subacute dyspnea associated with severe hypoxia noted to have bilateral corase crackles.
Her CXR demonstrated significant bilateral opacification with air bronchograms suggestive of consolidation. Difficult to tell if effusion was present.
PoCUS was employed to help differentiate whether this was a cardiogenic pulmonary edema versus non-cardiogenic pulmonary edema.
The final diagnosis was Influenza A.
Her CXR demonstrated significant bilateral opacification with air bronchograms suggestive of consolidation. Difficult to tell if effusion was present.
PoCUS was employed to help differentiate whether this was a cardiogenic pulmonary edema versus non-cardiogenic pulmonary edema.
The final diagnosis was Influenza A.

What parenchymal US findings would you expect for non-cardiogenic pulmonary edema?
Thoracic PoCUS revealed >3 B-lines diffusely with no evidence of asymmetry. Given this pattern, the differential remains quite wide. However, the absence and presence of other findings help narrow the list.
At Z4, there was no effusion. Its absence suggested this was unlikely cardiogenic pulmonary edema (some effusion would be expected with this magnitude of interstitial syndrome if it was due to CHF).
The linear probe was deployed to image the pleural line, it was noted to be coarse with notable segmental consolidation. This further narrows it down to an inflammatory process - most likely a pneumonia.
At Z4, there was no effusion. Its absence suggested this was unlikely cardiogenic pulmonary edema (some effusion would be expected with this magnitude of interstitial syndrome if it was due to CHF).
The linear probe was deployed to image the pleural line, it was noted to be coarse with notable segmental consolidation. This further narrows it down to an inflammatory process - most likely a pneumonia.
Case 7.
64M with known severe interstitial lung disease presented with acute on chronic shortness of breath.
How would ILD sonographic findings differ from cardiogenic pulmonary edema? (Click here for the answer)
How would ILD sonographic findings differ from cardiogenic pulmonary edema? (Click here for the answer)
Clip i.
Bilateral Z1-4 revealed significant number of B-lines. This is expected given the degree of fibrosis. The lung parenchyma is rendered much denser given the interstitial fibrosis.
Clip ii.
The B-lines are so dense in this case such that it is impossible to distinguish for discrete rays. It is as if they have coalesced together into one integrated ray with a "Search Light" appearance.
Clip iii.
The pleura is ragged and coarse, and B-lines can be seen arising from it.
Case 8.
45M presented with massive hemoptysis with no other clinical findings. The CXR was quite unremarkable barring mild opacification at the LLL
PoCUS was deployed in hope to localize the bleed, so that the patient maybe positioned in a lateral decubitus fashion whereby the culprit hemithorax would be placed dependently.
Before you scroll down for the answer, what are you looking for with the POCUS?
PoCUS was deployed in hope to localize the bleed, so that the patient maybe positioned in a lateral decubitus fashion whereby the culprit hemithorax would be placed dependently.
Before you scroll down for the answer, what are you looking for with the POCUS?

Clip i.
PoCUS revealed >2 B-lines seen at LZ4 - interstitial syndrome. Given the clinical context, the bleed is most likely originating from this region.
Clip ii.
Pleura evaluation with the linear probe revealed coarse and a ragged pleura indicating an inflammatory process - whether it be active or sequelae.
Take Home Messages:
- Interstitial Syndrome has quite a broad differential with similar PoCUS features
- Parenchymal PoCUS, in isolation, does not have sufficient discriminatory diagnostic power
- The clinical context weighs into the Clinical Synthesis